LongCovid and excess acidity/lactate theory - the positive feedback hyperinflammation loop by another name.
Interview by Gez Medinger with Vicky Van der Togt, a LongCovid patient, and Jeremy Rossman.
A video interview by Gez Medinger with Vicky Van der Togt, a LongCovid patient who worked to get better, and Jeremy Rossman, a researcher, was linked in a post by Dr Phillip McMillan. Vicky and Jeremy discuss excess acidity, lactate or lactic acid, as a treatable factor in LongCovid. When we exercise or lay in bed resting quietly, our mitochondria are still producing lactic acid and other oxidative stress chemicals and they need antioxidants to reduce the acidity - to reduce the amount of free radicals - positively charged chemicals.
A hydroxyl group has no charge when connected to other molecules -OH, but in a solution of water the hydrogen and hydroxyl group may separate into a free hydrogen proton with a positive charge -H+, and an oxygen hydrogen group with a negative charge, the oxygen is holding onto the other hydrogen’s electron (to complete the oxygen’s outer valence shell) with 8 electrons instead of 6). When a buffer solution is added to an acidic or basic solution the buffer chemical can accept either the excess negatively charged -OH- or positively charged -H+.
For health we need to maintain our body acid/alkaline level within a narrow range that is near neutral but slightly alkaline - 7.2 to 7.4 pH. This helpful introductory explanation is easy to follow and gets into how the acidity of a food doesn’t necessarily reflect how it will affect the acidity of the body after digestion: What Is The Ideal pH Of The Body?, By John Staughton, Last Updated On: 8 Jul 2022. (scienceabc.com)
Citrus fruits are acidic but complement our stomach acid and don’t increase overall body acidity, while diary products and meats aren’t ‘acidic’, but the waste produced during digestion is acidic and they result in a more acidic body after digestion. In general more produce, beans, nuts and seeds - magnesium foods, will help reduce acidity in the body. Inflammation of any type is increasing acidic waste products from the mitochondria or digestion. Whether LongCovid or other issues, chronic stress uses up B vitamins and magnesium and vitamin C in large amounts that standard food may not be able to provide. Many nutrients are needed and helpful too. When we have Nrf2, cysteine, glycine, and methionine, and are making enough glutathione for our mitochondria - its antioxidant power would b equivalent to around 300 oranges. We can’t eat 300 oranges every day but adequate protein can provide the amino acids needed to make glutathione and many phytonutrients and omega 3 fatty acids promote Nrf2.
Part one video: The Acid-Base Disruption Hypothesis for Long Covid | With Vicky Van der Togt and Jeremy Rossman, Gez Medinger.
An interesting point is >fluctuating lab values< asking a doctor to check acidity levels or lactate/lactic acid may lead to inconclusive “ normal”. Acidity levels vary with exertion and other factors and can vary in different parts of the body. Excess acidity is associated with chronic kidney disease.
A research study is being attempted with self-funding - donation and other resource links from the video comments:
Resources: The paper: https://www.frontiersin.org/articles/...
FAQ: https://researchaidnetworks.org/faq/
Lay summary: https://researchaidnetworks.org/hypot...
Audio version lay summary: • Hypothesis summar...
GoFundMe link: https://www.gofundme.com/f/donate-to-...
---- The Long Covid Handbook (Feb 2023) by Gez Medinger & Professor Danny Altmann (and published by Penguin Books) is now available in paperback, ebook and audiobook. A singular resource that brings together everything patients, clinicians and academics have learnt about the condition to date, as well as lessons from sufferers and researchers of ME/CFS and other chronic conditions. It offers world leading expert advice on understanding, managing and treating Long Covid. It is available from the following links. US: https://a.co/d/0gvkJCU UK: https://amzn.eu/d/9KjurGb (Youtube)
Part 2 of the interview video, Interventions for an Acid-Base Imbalance in Long Covid | With Vicky Van der Togt & Dr Jeremy Rossman, interview by Gez Medinger, is about treatment possibilities - What to do?
Vicky tried stuff and it helped but reminds the viewers that this is not proven, still a theory. Strategies she tried included strategies she found recommended for chronic kidney disease which can have acidosis as a symptom:
a) drinking a lot more water, with electrolytes added to it, to promote more urination and dumping of acidity;
b) a more alkalizing diet;
see my first post in the new How-To’s for Health section: Beans for breast cancer? and liver health? (substack).
& Alkalizing Foods that may help, other inflammatory food issues that may not. TRP channel activators, Lectin, Oxalates, Retinoic Acid, Histamine (pdf in my Dropbox)
c) breathing strategies, deep breaths rather than hyperventilating short compensatory breaths;
d) full range gentle exercise, stretching or other ways to promote lymphatic drainage throughout the body. Acidosis can collect in unused spots and be within normal ranges in areas that are in motion regularly.
Vicky mentioned that using bicarbonates can help acidosis but given intravenously can shift the body too far into the alkaline range and can be dangerous.
My use of it, sodium bicarbonate, is to add some of it, inexpensive Baking soda, to a glass of water. Just a dash or pinch, and drink to taste, good at first, then, oh, I had enough…, can be a gentle way to try sodium bicarbonate. In between meals rather than with meals as we need stomach acidity to digest. Apple cider vinegar or lemon or lime juice can aid meal digestion for older people who make less stomach acid typically.
Questions asked in the video ~ what is the underlying cause of the acidosis? Is the virus still there? as a low level or recurring infection?
I can answer the underlying cause of acidosis question - inhibition of Nrf2 leads to loss of glutathione production and a sudden need for 300 oranges a day worth of vitamin C or other antioxidants - to cope with normal needs, have some extra to deal with hyperinflammation too.
Indole-3-lactic acid is a postbiotic, tryptophan metabolite, which is protective of the intestine - when Nrf2 is present, but not in Nrf2 Knockout mice. (Zhang, et al., 2023)
Animal-based surgery with intestinal surgery as the injury: “Mechanistically, Indole-3-lactic acid (ILA) improved the expression of Yes Associated Protein (YAP) and Nuclear Factor erythroid 2-Related Factor 2 (Nrf2) after intestinal I/R. The YAP inhibitor verteporfin (VP) reversed the anti-inflammatory effect of ILA, both in vivo and in vitro. Additionally, we found that ILA failed to protect epithelial cells from oxidative stress in Nrf2 knockout mice under I/R injury.” (Zhang, et al., 2023)
ILA is a postbiotic known to be made by Bifidobacterium species, (Ehrlich, et al., 2020), Lactobacillus murinus (L. murinus), (Zhang, et al., 2023), and Lactiplantibacillus plantarum ZJ316 and other species of Lactilactobacillus. (Zhou, et al., 2022)
“ILA is one of the important tryptophan metabolites, mainly produced by Bifidobacterium in probiotic conditioned media [9]. Relatively high ILA yields of 22.17–33.12 mg/L were detected in Bifidobacterium infantis using liquid chromatography-tandem mass spectrometry (LC-MS/MS) [9]. Recent studies have demonstrated that species of Lactilactobacillus such as Ligilactobacillus salivarius, Lactiplantibacillus plantarum, Limosilactobacillus reuteri, Lacticaseibacillus paracasei and Lactilactobacillus sakei can also produce ILA at levels of 4.30–30.70 mg/L [10]. Lactilactobacillus are symbiotic bacteria found in the gut of healthy humans, helping to regulate the intestinal microbiota and activate the body’s immunity [11]. Especially in newborns aged 1–3 days, the intestinal microbiota are structurally single and dominated by Lactilactobacillus [12]. Could these Lactilactobacillus from the gut in early life also metabolize ILA to promote gut health?
The functional properties of ILA have been reported to mainly include free radical-scavenging activity, anti-inflammatory activity and immune regulation [13,14]. Walker et al. demonstrated that ILA metabolized by B. infantis in breast milk can suppress immune responses and promote the secretion of SCFAs by the intestinal microbiota, contributing to the prevention of necrotizing enterocolitis [15].” (Zhou, et al., 2022)
That clears things up - butyrate producing Bifidobacterium are needed to protect against SARS-CoV-2 and spike and they tend to be killed off by the chimeric biotoxin. Bubble drinkers for the win, again - eat zinc and resistant starch and Nrf2 promoting phytonutrients and polyphenols - in order to protect the microbiome and mitigate against spike effects on the microbiome. Good sunshine, blackout dark night, water, gentle movement, breathing, are also needs. There are many needs. Vicky states at one point that her strategies might sound simple (~not high tech or expensive) but that it wasn’t easy and that she took a slooowwwww approach - which is needed to reverse a positive feedback loop of inflammation. They mention that it seems a positive feedback loop and butyrate and polyphenols, niacin/tryptophan sparing, and other things can all help put a brake on the hyperinflammation loop.
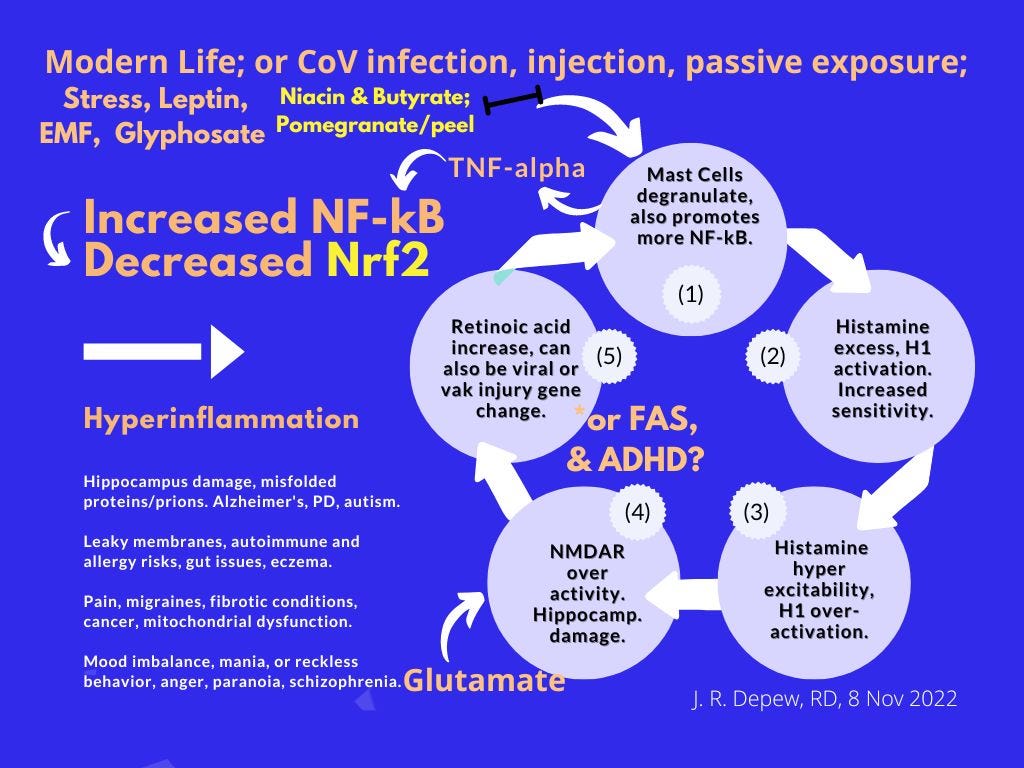
»Retinoid Toxicity - a new page, overactivation of vitamin A and carotenoids may be a factor in LongCovid, for similar reasons to ME/CFS following an Epstein-Barr viral infection. If carotenoids and vitamin A are being over-activated to Retinoic acid, then chronic inflammation and acidosis would be likely from the inhibition of Nrf2 and increase in oxidative stress chemicals.
Disclaimer: This information is being shared for educational purposes within the guidelines of Fair Use and is not intended to provide individual health guidance.
Reference List
(Ehrlich, et al., 2020) Ehrlich AM, Pacheco AR, Henrick BM, Taft D, Xu G, Huda MN, et al., Indole-3-lactic acid associated with Bifidobacterium-dominated microbiota significantly decreases inflammation in intestinal epithelial cells. BMC Microbiol. 2020 Nov 23;20(1):357. doi: 10.1186/s12866-020-02023-y. PMID: 33225894; PMCID: PMC7681996. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7681996/
(Zhang, et al., 2023) Zhang, FL., Chen, XW., Wang, YF. et al. Microbiota-derived tryptophan metabolites indole-3-lactic acid is associated with intestinal ischemia/reperfusion injury via positive regulation of YAP and Nrf2. J Transl Med 21, 264 (2023). https://doi.org/10.1186/s12967-023-04109-3 https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-04109-3
(Zhou, et al., 2022) Zhou Q, Xie Z, Wu D, Liu L, Shi Y, Li P, Gu Q. The Effect of Indole-3-Lactic Acid from Lactiplantibacillus plantarum ZJ316 on Human Intestinal Microbiota In Vitro. Foods. 2022 Oct 21;11(20):3302. doi: 10.3390/foods11203302. PMCID: PMC9601829. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9601829/





There'd have to be substantial renal and lung damage before this stopped working: CO2 + H2O <-> H2Co3 <-> H+ + HCO3
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4670772/#fd2