Ototoxicity, part 2
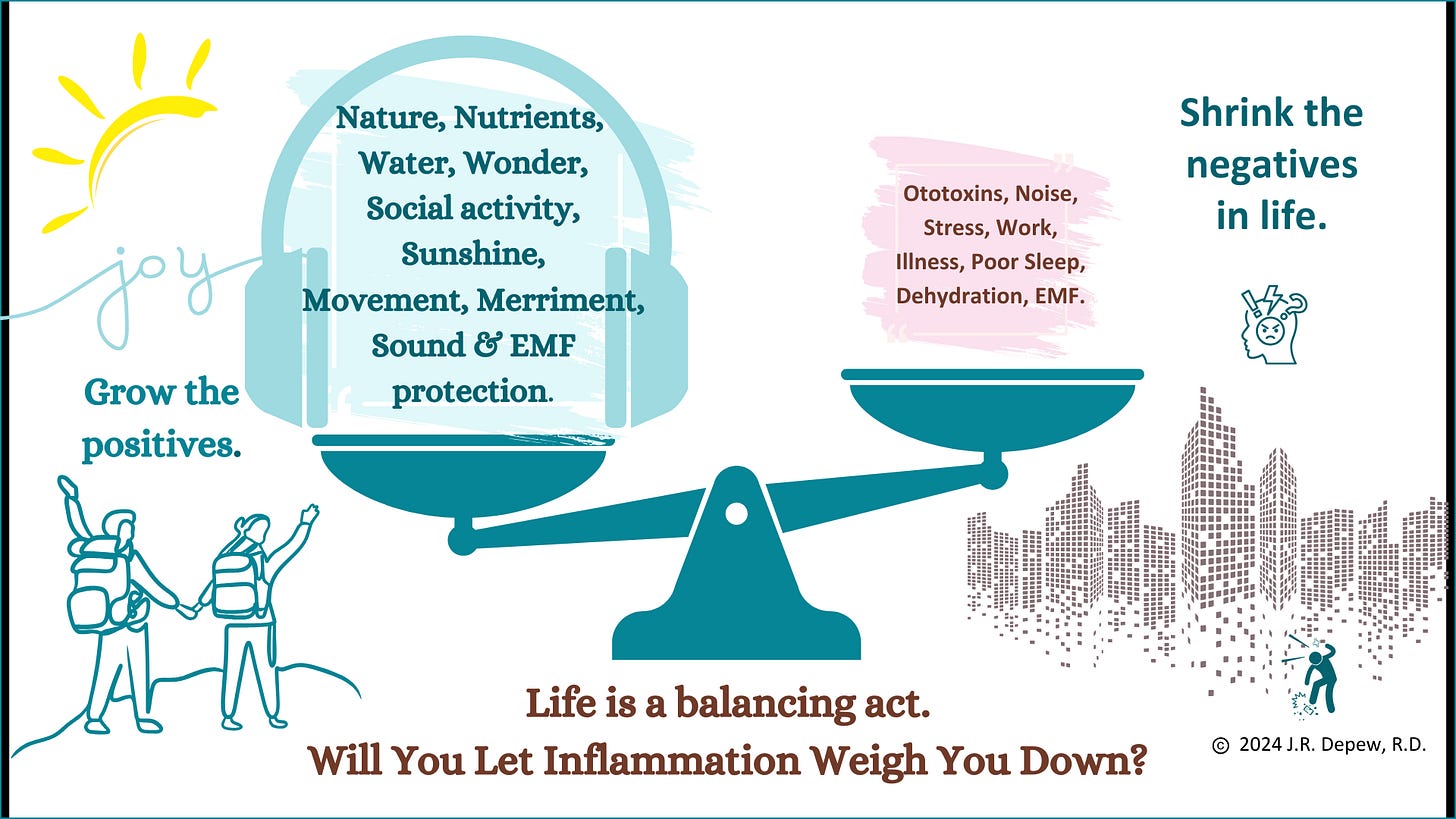
Any emotional or physical stressor would add to the body load of oxidative stress and add to a risk of a positive hyperinflammation loop occurring if we run out of antioxidants, polyphenols, vitamins and trace minerals for detoxing the oxidative stress waste chemicals. At the end of the day’s campfire, we need to put out the smoldering coals, or risk burning down the building overnight (roughly).
Nutrient deficiency, excess physical stress (loud noise), or ototoxins, might be tolerable separately but put them all together and chronic damage can be the result.
Our hearing involves motion sensing “Hair Cells” which don’t regrow if damaged as they can in other species like birds. Genetic study of the specialized cells in chicks has led to treatment options for promoting regrowth of Hair Cells in humans. Caspase enzyme inhibitors may help restore the regeneration potential – which supports the use of pomegranate peel extract, more on that later.
Many factors are involved in hair growth on our head – (Substack) – but Hair Cells in our inner ears are simply called that because they stick up and wave back and forth with changes in our motion or from the motion of sound waves transmitted through the fluid within the snail shell shaped cochlea of our inner ear. Many of the same factors and nutrients affecting our body hair would also impact our inner ears though.
Oxidative stress from any source is damaging throughout the body.

Mitochondrial dysfunction increases oxidative stress and leads to more mitochondrial dysfunction… which increases oxidative stress and leads to more mitochondrial dysfunction which increases oxidative stress and leads to… you see the loop.
Oxidative stress and mitochondrial dysfunction tips us towards more acidity, and that may increase accumulation of salicylates from pain-relievers or other medication use, mint lozenges and toothpaste, minty topical pain-relieving ointments, or spices in the diet. We detoxify salicylates less well if overly acidic, lacking in glycine, and/or genetically susceptible and low in methyl folate. Salicylates are a known ototoxin and salicylate excess or sensitivity is often misdiagnosed as something else, leaving the underlying problem continuing to cause damage.
Many commonly used medications may have ototoxic, hearing damaging effects due to depleting mitochondrial support nutrients: (List in this post; or see A Disturbingly Transparent Table: post) My list of nutrients that may be at risk for deficiency or imbalance in mitochondrial dysfunction, schizophrenia, Alzheimer’s dementia, Parkinson’s or Huntington’s disease, and tend to be depleted by psychiatric medications - was begun in this post. The Table is in my pomegranate paper.
Dehydration is a big risk to the inner ear and lack of magnesium is part of that, or lack of potassium in ratio to sodium. Salt is not ‘bad’, so much as lack of potassium plus excess sodium is bad. Salt used to be valued like a currency… or a commodity, oh, it still is. It is just readily available now, rather than being on a camel train slowly traveling towards us.
Ototoxins - substances known to harm hearing or the inner ear hair cells.
Nutrients: Inflammation in general causes an increased use and loss of nutrients while also increasing the need for nutrients to help detoxify waste chemicals. The standard US diet can add to the risk of low levels of magnesium, B vitamins and other nutrients needed for hearing and general health.
Noise and Vibration: Physical stress adds to toxin loads for our body’s clean-up methods. Noise is a physical stressor. Living next to a train station or other load traffic or industrial area will add to an inflammatory burden and increase risk of degenerative disease. Those apartments are inexpensive because no one wants to live there.
During my travels camping in my car, I could park anywhere, put up my window privacy panels and sleep… unless a security guard tapped on my window (that happened a couple times when I chose the wrong parking lot). It was quite liberating and sleeping near eucalyptus trees is wonderful smelling. BUT I found I could not sleep in an industrial area that had a humming vibratory noise. I hadn’t noticed the noise during the day, being inside the building muffled the noise or vibratory feeling. It was not loud until laying there in the dark and there was a throbbing odd beat. I moved my car. I could not sleep there. I had rented a shared space office desk nearby so I had many opportunities to notice the very low throbbing feel more than a noise. It was present all day outside, just not very noticeable and not inside. Some factory in the area had generators going all the time or intermittently turning on.
…That means that having an office or working outdoors in the industrial setting could be adding to your body’s stress load all day long and you just don’t notice because you’re busy working instead of trying to sleep. Laying there at night trying to sleep, I did notice the low throbbing sensation. That vibratory noise would be causing inflammation within the body whether you’re sleeping or awake though.
The combination of stress, nutrient deficiency and ototoxins can lead to the worst risks to our hearing and balance.
Physical or emotional stressors use up nutrients and increase need for extra nutrients. It is a combination of problems. But wait! Reverse that…. and Le Prell, et al., 2011 found that a “Nutrient-enhanced diet reduces noise-induced damage to the inner ear and hearing loss.” (Le Prell, et al., 2011)
The addition of just four nutrients, β-carotene (Vit. A precursor), vitamin C (ascorbic acid), vitamin E (alpha-tocopherol), and magnesium, was found protective (higher supplemented Diet B) in an animal-based study on noise-induced hearing damage. Hair Cells were still damaged by the noise but loss of Type II fibrocytes was reduced significantly with the supplemented diet compared to standard lab animal control diet. For 28 days prior to loud noise exposure, supplemented animals were given a diet with 9 times more magnesium, 16 times more beta-carotene, 53 times more vitamin E and 3600 times more vitamin C. Rodents can make their own vitamin C so typically are not given it in standard lab kibble, any is more than zero. (Le Prell, et al., 2011)
*Not needed here, but an online converter for calculating what an animal dose would be for a human can be found here: ‘Animal to Human Dose Calculator,’ (acmeresearchlabs.in)
*Mice eat ~ 6-20 grams of food per day varying from more during active growth to less in the stable adult phase of life, (Brave AI), so they would be getting a small amount of food but with an increased concentration of the supplemented nutrients.
But… those are all mega-dose levels of supplementation. We can take it to suggest that adequacy will help protect hearing, and deficiency won’t.
TD.07213 “Control” TD. 07506 “Diet B”
Magnesium1 (mg/kg chow) 500 4500
Beta-carotene2 (mg/kg chow) 14 224
Ascorbic acid3 (mg/kg chow) 0 3600
Alpha-tocopherol3 (mg/kg chow) 50 2650 (Le Prell, et al., 2011)
Vitamin A recommendations for adults 19 years and older:
Men: 900 mcg retinol activity equivalents (RAE) per day (equivalent to 3,000 International Units (IU))
Women: 700 mcg RAE per day (equivalent to 2,333 IU)
Vitamin A: Multiplying the RDA by 16 (Le Prell, et al., 2011) might give 11000 to 15000 mcg RAE of beta-carotene per day which could get into toxicity levels in a person not processing it well. Taurine adequacy is important for the body to cope with activated Retinoids.
Taurine – Brave AI is enthusiastic about taurine for ending tinnitus and helping during hearing loss.
Causal factor: Retinoid Toxicity – excess activated vitamin A. Taurine being so helpful against tinnitus and hearing loss suggests that Retinoid Toxicity is a cause of tinnitus and hearing problems for those responding to taurine. So mega-doses of vitamin A or beta-carotene would make those people’s hearing symptoms worse, while taking taurine or increasing red meat in the diet helps the body to deactivate Retinoic Acid. Brave AI calls Retinoid Toxicity ototoxic. And tinnitus or other hearing issues are known side effects of the retinoid medication Accutane. Alopecia is too. (dailymed.nlm.nih.gov) SARS-CoV-2 or chimeric spike effects may be in play in our current times then. It is possible that a gene change in the liver is promoted which leads to retinoids being activated which leads to epithelial and endothelial cell differentiation and SARS-CoV2 likes to colonize endothelial cells. Epstein Barr Virus likes to colonize epithelial cells and the Retinoic Acid mechanism has been studied for that type of infection. See this post.
If excess activated vitamin A is a causal factor, then a diet quite low in vitamin A and beta-carotene would be helpful, along with taurine supplementation or an increase in red meat intake. Supplement, ~ 2-3 grams twice a day is generally considered a safe amount.
Plenty of sunshine also helps the body use up stored vitamin A and adequate vitamin D levels is protective of hearing.
Excess sunshine however, skin damaging levels, may increase risk of hearing loss and a lack of antioxidants increased the association. (Michikawa, et al., 2013)
Vitamin C – is a pro-oxidant if taken in excess. Someone who is ill and inflamed would need more than someone using it for prevention purposes. Excess supplementation with vitamin C can add to an over-acidity problem in the body if more is taken regularly than was needed. Symptoms of gout toe pain or elevated Uric Acid labs would be indicators to supplement with no more than 250 mg of vitamin C per day.
Magnesium – adequacy of magnesium is protective against tinnitus (Cevette, et al., 2011) and topical sources might be helpful if oral supplementations haven’t seemed to help. An unhealthy gut tends to dump magnesium and an overly acidic body or a large calcium load can lead to more loss of magnesium by the kidneys. Magnesium helps in many ways.
Magnesium and Cochlear Hair Cells (Brave AI summary)
Cochlear hair cells are the sensory receptors responsible for converting sound waves into electrical signals in the inner ear. Magnesium (Mg) plays a crucial role in maintaining the health and function of these cells, particularly in response to noise-induced hearing loss (NIHL).
Mechanisms of Magnesium Action
Calcium channel regulation: Magnesium inhibits the influx of excessive calcium ions (Ca2+) into cochlear hair cells, which can lead to cell damage and death. By regulating calcium channels, magnesium helps maintain a balanced ionic environment and reduces oxidative stress.
ROS reduction: Magnesium has antioxidant properties, which help reduce reactive oxygen species (ROS) formation in cochlear hair cells. ROS accumulation contributes to NIHL by damaging hair cells and disrupting their function.
Energy metabolism: Magnesium is essential for energy production in cochlear hair cells, particularly in the mitochondria. It helps maintain ATP levels, which are critical for maintaining hair cell function and survival.
Cell signaling: Magnesium modulates various signaling pathways involved in cochlear hair cell function, including the NMDA receptor-mediated excitotoxicity and the regulation of glutamate release. *See the first post for a lot more on this risk for hearing or brain damage. (Ototoxicity-Part 1)
Studies Supporting Magnesium’s Role
Reduced noise-induced hearing loss: Studies have shown that magnesium supplementation can reduce NIHL in animal models, likely due to its antioxidant and calcium channel-regulating effects.
Protection of hair cells: Magnesium has been shown to protect cochlear hair cells from damage caused by noise exposure, oxidative stress, and ototoxicants.
Preservation of cochlear function: Magnesium has been found to preserve cochlear function and reduce hearing threshold shifts in noise-exposed animals.
Clinical Relevance
While magnesium’s role in cochlear hair cells is primarily studied in animal models, its potential therapeutic applications for NIHL and other hearing disorders are promising. Magnesium supplementation or magnesium-rich diets may help protect cochlear hair cells and preserve hearing function in individuals exposed to noise or at risk of hearing loss. (Brave AI summary)
Schizophrenia – the nutrient deficiencies or imbalances that are involved as possible causal factors show overlap with those involved in hearing loss or tinnitus.
As I looked into these nutrients that seem related to hearing health, the list seemed to overlap with my list of factors that may be involved in symptoms resembling schizophrenia. (Substack) Checking comorbidity, I find there is a strong overlap between schizophrenia and tinnitus or hearing loss.
NMDA receptor activity may be a link. (Brave AI summary) See the prior Part 1-Ototoxicity post for more details - later risk of dementia is also part of the comorbidity pattern. Mitochondrial dysfunction is an underlying commonality.
If interested in schizophrenia, the biochemistry of adrenochrome clearance is pertinent - see this post.
Hearing impairment is related to later risk for schizophrenia or hallucinations and psychosis.
Reduced social interaction - isolation due to poor hearing may be a factor - but oxidative stress overload and nutrient deficiency might be worsening hearing and causing cognitive damages at the same time.
“Hearing impairment increases the risk of hallucinations and/or delusions in adults.
Hearing impairment early in life increases the risk of later schizophrenia.
Elderly patients with impaired hearing have an elevated risk of developing delirium.
Interpersonal, neurocognitive, and neurobiological processes may be involved.
Diagnosis and treatment of impaired hearing may lower psychosis risk.” (Linszen, et al., 2016)
More nutrients that seem protective of our hearing, and our brain and mitochondria:
Vitamin E – an antioxidant, adequacy may be protective for hearing. Supplementation with vitamin E was found beneficial or inconclusive in various studies on hearing. B12, folic acid, and N-acetyl cysteine supplementation was more conclusively helpful. (Brave AI Summary) I would always recommend use of methyl folate rather than inactive folic acid though.
Folate or Folic acid – deficiency has been firmly linked to hearing loss and supplementation of either form of the B vitamin shows protective benefits. (Brave AI summary)
Vitamin B12 deficiency has been associated with cochlear dysfunction in the ear. (Karli, et al., 2013)
Zinc deficiency may also be causal for hearing loss. The cochlear and vestibular soft tissue is particularly concentrated in zinc compared to the other tissues of the body. (Shambaugh, 1986) Zinc supplements help when deficiency is a concern but don’t provide help if not needed, healthyhearing.com.
Omega 3 fatty acids, Vinpocetine, Ginseng, and Coenzyme Q10 may be helpful supplements for hearing loss or prevention, healthyhearing.com.
Betaine, TMG, or DMG, dimethylglycine – adequacy is anti-inflammatory. (Lendvai, et al., 2023) We need glycine, cysteine and glutamic acid to make glutathione, our body’s main antioxidant.
Methionine – preloading with methionine prior to noise exposure was protective. (Brave AI summary) Methionine and glycine are used in our methylation cycles.
Iodine – there is a strong link between iodine deficiency or hypothyroidism and hearing loss. Risk seems to be worse if the iodine deficiency occurs during child development. (Brave AI summary)
Selenium – also seems to have a strong link to hearing protection but iodine had more results. (Brave AI summary)
Alpha Lipoic Acid (ALA) – an antioxidant that supports methylation and mitochondrial function. It has shown benefits as an injected treatment for hearing loss, “Intratympanic Alpha-Lipoic Acid Injection”. (Han, et al., 2022) ALA has less pro-oxidant risks than vitamin C.
B vitamin Para-aminobenzoic acid (PABA)? B vitamin, PABA, may have pain-relieving potential due to inhibition of TRPA1 and TRPV4 ion channels. (Bang, et al., 2012) *Part 1 discussed TRP channels in detail, and more on TRPA1 channels is planned for Part 3. Supplements of 100-500 mg or a gram of PABA per day would likely be safe. It is a water-soluble B vitamin but it does not have an official guideline for PABA, also known as vitamin B10. Over 12 grams daily may lead to toxicity symptoms.
Any emotional or physical stressor would add to the body load of oxidative stress and add to a risk of a positive hyperinflammation loop occurring if we run out of antioxidants, polyphenols, vitamins and trace minerals for detoxing the oxidative stress waste chemicals. At the end of the day’s campfire, we need to put out the smoldering coals, or risk burning down the building overnight (roughly).

Ototoxins:
Some medications and toxins are known to specifically cause damage to the Hair Cells of the inner ear or other aspects involved in hearing. The inner ear has the motion sensing Hair Cells in the snail shaped cochlea where they sense the motion of sound waves being amplified by the eardrum, the tympanic membrane. The motion sensing Hair Cells are also found within the urticle of vestibular system of the inner ear where they sense the motion of our head and body as we move around. Eye sight and visual tracking of something like a bird or plane moving through the air can also be affected by damage to the vestibular system’s Hair Cells. You might be able to hit a still target, but not be able to do skeet shooting anymore.
Medications known to have ototoxic effects include common antibiotics, aspirin and NSAID pain-relievers, certain diuretics, some cancer or anti-cancer treatments, and occupational toxins including lead and carbon monoxide. Risk increases with the combination of an ototoxic medication and ototoxic environmental exposure to heavy metals or carbon monoxide, which might simply be living in a city with bad urban smog conditions and taking pain-killers regularly for your headaches add an antibiotic or diuretic with ototoxic risks and you may be left in silence – deaf, or with annoying tinnitus buzzing in your head.
“The International Ototoxicity Management Group (IOMG) is a global consortium created to address a gap in healthcare regarding the treatment of individuals who experience hearing difficulties following the administration of ototoxic medications or exposure to ototoxicants in the environment.” en.wikiversity.org;
Recent publications by IOMG can be downloaded here: ncrar.research.va.gov.
Known Ototoxins
Antibiotics:
Aminoglycoside antibiotics (no longer commonly used): Gentamicin, Streptomycin, Tobramycin, Kanamycin*, (emedicine.medscape.com), Neomycin
Fluoroquinolones: Ciprofloxacin, Levofloxacin
Macrolide antibiotics: Erythromycin, Azithromycin, *Risk of tinnitus occurring is more likely with extended use rather than a short-term use.
Nonsteroidal anti-inflammatory drugs (NSAIDs):
Salicylates: Aspirin, Acetylsalicylic acid (ASA), Methylsalicylates (e.g., methyl salicylate, oil of wintergreen)
Other NSAIDs: Ibuprofen, Naproxen, Ketoprofen
Phytonutrient antioxidants function as COX2 inhibitors and supplement size doses may be additive for a salicylate sensitivity or excess.
Hypertension/heart disease:
ACE inhibitors, Angiotensin-converting enzyme (ACE): Lisinopril (Zestril), Enalapril (Vasotec), Ramipril (Altace)
Beta-Blockers for hypertension or coronary artery disease: Metoprolol (Lopressor, Toprol XL), Bisoprolol, Nebivolol (Bystolic).
Diuretics:
Loop diuretics: Furosemide, Bumetanide, Torsemide
Chemotherapy agents:
Platinum-based agents: Cisplatin, Carboplatin, Oxaliplatin
Anticancer drugs: Asparaginase, Bleomycin, Doxorubicin
Retinoid medications:
Accutane - typically used for cosmetic or acne purposes.
Acne is likely dysbiosis of the skin microbiome and/or dysbiosis of the gut-brain-skin axis. (Lee, et al., 2019) Pomegranate peel extract has been shown effective for acne, reducing Staph and the skin microbiome. (news-medical.net; D’Arcangelo, et al., 2024)
Topical Retinoid medications may be used for cancer treatment, acne, or other skin conditions: Tretinoin (all-trans retinoic acid), Adapalene, Tazarotene, Trifarotene, Alitretinoin, and Bexarotene
Approved indications: Acne vulgaris, psoriasis, photoaging/rhytides, cutaneous T-cell lymphoma, and Kaposi’s sarcoma.
Off-label uses: Keratosis pilaris and hyperpigmentation
Oral Retinoids: Isotretinoin; Available by prescription for severe acne.
Mechanism of action: Inhibits sebaceous gland activity, reducing sebum production.
Side effects: Common: dry mouth, nosebleeds, and increased triglycerides; Rare: liver damage, depression, and suicidal thoughts. <« and you thought acne was your problem…
Other substances with Ototoxic risk:
Quinine medications: Quinine (antimalarial), Hydroxychloroquine
Environmental and occupational chemicals: Mercury, Tin, Lead, Carbon monoxide, Certain solvents and heavy metals.
Sars CoV2 or chimeric spike injections seem to be an ototoxins, directly harmful to the hair cells needed for our hearing and our sense of balance and ability to visually track, to focus on a bird flying by smoothly instead of the eyes jerkily trying to keep up and shift ahead along the flight path. It may affect the coil like ankyrin repeat domain of TRPA1 channels, which are involved in the mechanical transmission of sound from the hair cell to its pore. See Part 3 (in the works).
Ototoxic medication lists, (Brave AI summary):
longislandaudiology.com, Long Island Audiology - Ototoxic Medications List
soundrelief.com, List of Ototoxic Medications - Sound Relief Hearing Center
emedicine.medscape.com, Ototoxicity: Overview, Aminoglycosides, Other Antibiotics
Also, 12 Medications That May Cause Tinnitus (Ringing in the Ears), by Tegan Smedley, PharmD, APh, Reviewed by Karen Hovav, MD, FAAP, Updated Aug 20, 2024, goodrx.com.
Ototoxicity overview:
my.clevelandclinic.org, Ototoxicity: Symptoms, Causes & Treatment
webmd.com, What Is Ototoxicity? Learn About Causes, Symptoms, and More,
Post too long for email, I will continue with more details about the role of TRPA1 channels in hearing in a Part 3 post.
Disclaimer: This information is being provided for educational purposes within the guidelines of Fair Use and is not intended to provide individual health care guidance.