Not brief review of nutrient deficiencies that might cause Neural Tube Defects, and why folic acid might help a little even with it not being methylated.
It was brief when I got started. Too long for email. /Included: methyl folate & B12, choline, B2, B6, zinc, betaine, Dimethylglycine. Purine Nucleotides. Iron, iodine, prenatal vitamins & tolerance.
This was meant to be a ‘Brief folate in prenatal health review’, however I learned of other nutrient deficiencies involved in Neural Tube Defects. Zinc, choline, and B12 deficiencies have also been associated with Neural Tube Defects and elevated homocysteine which is seen in some types of methylation gene differences.
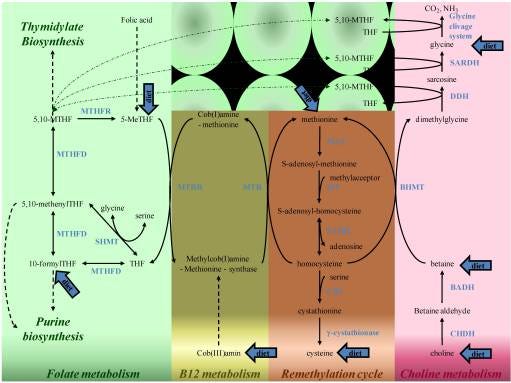
Gene differences in methylation cycles impacting a few nutrients and blocking methylation cycle function probably does seem to be involved, based on animal studies showing that blocking methylation cycles causes NTDs. (Imbard, Benoist, Blom, 2013) That might make methyl folate and methyl B12 a need, but choline or betaine or Dimethylglycine or riboflavin or bioactive B6 might also be what the person needs in amounts greater than typical foods provide - depending on which gene alleles they have.
Why does folic acid help though? It wouldn’t help if zinc deficiency is the cause of the NTD but if there was a lack of purine nucleotides, then folic acid could be used to make those, without needing to be methylated first. (Imbard, Benoist, Blom, 2013)
Having recently written a post about a new review article about folic acid recommendations in prenatal care - I wanted to reiterate that the recommendations for folic acid prenatally are likely wrong for the most at-risk mothers and infants if folate is what is needed. Folic acid would not help compared to the help that methyl folate might provide or more individually, look at other nutrients which might be needed due to the person’s specific gene differences in the methylation cycles.
See Table 2 and Figure 4 for gene alleles associated with Neural Tube Defects. (Imbard, Benoist, Blom, 2013) I have one of them but must have done okay with my riboflavin and folate intake, and not overheating while pregnant, because my kids are okay. At hotter temperatures, slightly hotter body temperature, my MTHFR 677C > T gene allele doesn’t work as well (allele rs1801133). I need to stay cool for better energy level - and yes, I agree, I don’t like a hot sunny day at the beach for more than 20 minutes. I prefer to work outside in early morning or cooler evening temperatures.
The previous post: Folate or Folic acid, pre-conception to week 5-8 prenatally, may reduce NTDS & autism risk. Recent review report by the US Preventive Services Task Force. And, lean muscle mass is protective against Alzheimer's risk. (Substack)
The main point - folic acid is recommended for all women of child-bearing years at 400 or 800 mcg per day as a precaution. Neural tube defects (NTD) occur very early in pregnancy, often before a woman might know she is pregnant at about week three to four. Having healthy habits and nutrient intake prior to conception is important and something I certainly promote too. However, a certain percentage of the population can’t methylate folic acid to a usable form - AND those are the people who are most likely going to have neural tube defects in their infants.
Folic acid supplementation is the standard recommendation to reduce NTD risk, however, how exactly folic acid helps is not known. (Imbard, Benoist, Blom, 2013) Probably because it isn’t the folic acid that helps, it is only likely to help after being methylated by a person whose genes allow remethylation of folate.
“Neural tube defects (NTDs) are common complex congenital malformations resulting from failure of the neural tube closure during embryogenesis. It is established that folic acid supplementation decreases the prevalence of NTDs, which has led to national public health policies regarding folic acid. To date, animal studies have not provided sufficient information to establish the metabolic and/or genomic mechanism(s) underlying human folic acid responsiveness in NTDs.” (Imbard, Benoist, Blom, 2013)
Neural tube defects range from cleft palate or brain issues at one end of the spine and spina bifida risk along the developing spinal cord. Within the fetus the neural tube is formed from a fold in the neural crest end of the ball of cells, which then becomes the spinal cord and brain - so we want it to develop normally. Brief video animation of neural tube formation in an embryo: General Embryology - Detailed Animation On Neurulation, Medical Animations (Youtube).
The current recommendation is that if someone has a history of a prior pregnancy with an NTD then they are recommended to take a mega dose of folic acid - as if more of a non-helpful thing is going to help even more than a smaller amount of a non-helpful thing.
Folic acid in small or large amounts is dumping a box of puzzle pieces that don’t fit right into a box of puzzle pieces that will complete a puzzle if assembled correctly. Throwing in an additional 400-800 bad puzzle pieces will make it harder to find any correctly fitting pieces. Throwing in an additional 4000 bad puzzle pieces will make the task ten times more difficult. Mega-doses of folic acid don’t really help anyone else either because they all would need to be methylated before they would be able to donate a methyl group, which is the job of folate.
If you have a flat tire and you need to change it, is it helpful to have a spare tire that is also flat? Is it 4000 times more helpful to have 4000 flat spare tires? No, that would not be helpful at all. You would be drowning in flat spare tires.
Summary point - if your doctor is insisting on a prenatal vitamin because of the risk of neural tube defects, just look for a methyl version of a good quality one-a-day and it should contain 400 mcg of folate and ~ 500 mcg of methyl cobalamin (B12).
Methyl B12 and other targeted nutrients may be needed due to gene alleles within methylation cycle pathways.
Folate deficiency alone has not been shown to cause NTDs in animal studies, but it did cause reduced size (intrauterine growth retardation). Other nutrient deficiencies must be involved too. Lack of B12 or choline or excess of homocysteine have been linked to risk of neural tube defects. Animal studies have shown that inhibiting the methylation cycles does cause Neural tube defects, and without other anomalies or growth retardation. Providing methionine helped in some of the knockout mice gene dysfunction studies. Animal studies on elevated homocysteine prenatally have had mixed results regarding risk of NTDs. (Imbard, Benoist, Blom, 2013) Other studies report low choline is the risk, I am wondering if that was a typo in the Abstract.
Folate might also be helping by formation of nucleotides, see the section on purines below. (Imbard, Benoist, Blom, 2013)
The information on the varied nutrients that may help reduce risk of NTDs suggests that women with gene differences in the methylation cycle pathways are more at risk for not providing their baby with adequate methylated folate and B12, and the issue may not be related only to folic acid or folate. It might be lack of bioactive B6 or B12 or other B vitamins, or zinc* (*last section of the post).
“However, several lines of evidence suggest that not only folates but also choline, B12 and methylation metabolisms are involved in NTDs. Decreased B12 vitamin and increased […*] homocysteine in maternal blood have been shown to be associated with increased NTDs risk. Several polymorphisms of genes involved in these pathways have also been implicated in risk of development of NTDs. This raises the question whether supplementation with B12 vitamin, betaine or other methylation donors in addition to folic acid periconceptional supplementation will further reduce NTD risk.” (Imbard, Benoist, Blom, 2013)
[…*] *The Abstract mentions ‘increased total choline’ but the text of the article mentions low choline were observed and other sources do to.
Excess homocysteine can be inflammatory and can occur with various gene alleles affecting methylation cycle pathways. Choline metabolism is also part of the cycles - flashback to the last post - choline can be made into the methyl donor betaine which then becomes dimethylglycine if your BHMT gene is functional, and you have adequate protein in your diet to make a good supply of enzymes.
“Over the years, more and more studies suggest that not only folate but whole methylation metabolism could be involved in the etiology of NTDs. This review will focus on the involvement of methylation metabolism in the onset of neural tube defects.” (Imbard, Benoist, Blom, 2013)
Low choline prenatally has more often been associated with neural tube defects according to this review (Irvine, et al., 2022) and risk may be 2.4 times greater for women with the lowest levels of choline. (Digitale, med.Stanford.edu/news) Egg yolk (not the white) is a good source of choline. Vegans likely need to supplement with choline and methyl B12 and vegetarians may need to also.
“Two nutrients in particular, folate and choline, have been linked to the prevention of neural tube defects and to both health and cognitive outcomes in children [9,22,23,24,25,26].” (Irvine, et al., 2022)
“Risk for neural tube defects was 2.4 times higher in women with the lowest blood choline levels compared to women with average blood choline levels. The highest blood choline levels were associated with the lowest risk.” (Digitale, med.Stanford.edu/news)
Betaine supplementation along with B12 is considered by (Imbard, Benoist, Blom, 2013) or other methylation donors - however, it really depends on the person’s gene differences. Betaine would make my queasy as it is the conversion of betaine to dimethylglycine (DMG) that I can’t perform as well as normal. I need DMG to keep things chugging along the cycles smoothly. That also may leave me low in choline and with elevated homocysteine as BHMT enzyme is needed reform methionine from homocysteine.
The graphic does help (last post) - we can see that vitamin B6 and B12 are needed to keep steps of the methylation cycle going. Vitamin B12 is needed for folate to donate a methyl group to homocysteine to restore methionine. Vitamin B6 is needed to change some of the homocysteine into cysteine which might be used to make the antioxidant glutathione (GSH) (not shown in this smaller graphic) in the transsulfuration cycle which also produces “the gaseous signaling molecule hydrogen sulfide (H2S)”. (Sbodio, Snyder, Paul, 2018)

Purine formation and nucleotides.
Vegans have less or no preformed nucleotides in their diet unlike someone who eats meat or sardines. Nutritional yeast flakes are a source of nucleotides. It takes 14 enzymatic steps to make a nucleotide and we need 100s of nucleotides to make each strand of RNA or DNA.
Folate can be used to make purines which are used in nucleotides. If we are trying to grow new cells for a baby or for our own healing, then we need nucleotides to make strands of messenger RNA. The mRNA will then be used to make a protein which might be an enzyme or receptor or other cell part. Purines in DNA include adenine and guanine. Aside: “The pyrimidines in DNA are cytosine and thymine; in RNA, they are cytosine and uracil.” (albert.io)
Iodine - 250 mcg a day minimally for prenatal and lactation stages of life.
An additional iodine or trace mineral supplement might be needed too. A multivitamin by Thorne ‘Basic Nutrients 2/Day’ that I use for my mother contains 400 mcg L-5-methyltetrahydrofolate and an additional 267 mcg of another form of folate, and 600 mcg of methylcobalamin. It only has 75 mcg of iodine though (and that is in 2 capsules a day, take at breakfast and dinner ideally to maximize availability to the body.)
Iron - constipating supplements or bioavailable Moringa leaf?
The question of the indigestible 18 mg of iron in prenatal vitamins is another question. Someone who is losing blood needs higher doses, along with more protein and B vitamins and magnesium to grow more blood cells, but otherwise, eating good food sources of iron will provide more bioavailable iron and be less indigestible.
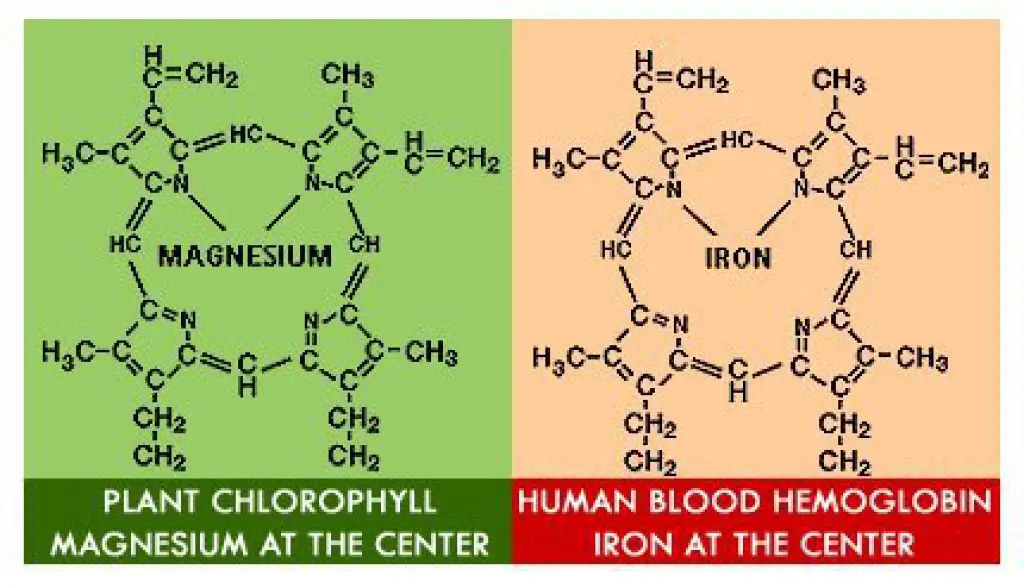
Popeye was not wrong about eating spinach for strength. It has iron and magnesium and B vitamins and vitamin A and C. So would other greens - it doesn’t have to be spinach. Chlorophyll is chemically similar to hemoglobin but it has atoms of magnesium instead of iron. It would be providing the building blocks needed to make the protein portion of hemoglobin though.
Deep green vegetables, leafy greens, are a good source of iron and the vitamin C which can help its absorption from plant sources, however it is not equally as well absorbed depending on other phytonutrients in the plant. Moringa leaves were found to be the most bioavailable iron out of a few types of tested green leafy vegetables. (Amagloh, et al., 2017) *study based in Ghana.
Product example: Moringa Leaf Powder/Mountain Rose Herbs, nice write up, I am unaffiliated with the company but have found their service and products to be excellent. I was using Moringa powder in my dad’s chocolate porridge every morning.
My Prenatal/Child page on jenniferdepew.com goes into supplement choices and issues for general prenatal care and has information for CoV or other infection care with the Basic Stack and Extended Stack of things that might help - pick some. It is a list of choices within categories, for the most part.
Zinc deficiency prenatally is also a cause of Neural Tube Defects. (Li, Zhang, Niswander, 2018)
The mechanism of action seems to be apoptosis/death of cells that should have been growing to close the open fold of the neural tube. It generally closes/grows together from the center of the spine first, so a neural tube defect might include an opening at the tail end of the spine (spina bifida) and some other defect at the jaw or brain end of the neural tube fold.
If you are taping a package closed and only have one piece of tape at the center, both edges will remain open. You need three pieces of tape along that edge of the wrapping paper.
[Mouse] “Embryos cultured with the zinc chelator TPEN failed to close the neural tube and showed excess apoptosis. TPEN-induced p53 protein stabilization in vivo and in neuroepithelial cell cultures and apoptosis was dependent on p53. Mechanistically, zinc deficiency resulted in disrupted interaction between p53 and the zinc-dependent E3 ubiquitin ligase Mdm2, and greatly reduced p53 ubiquitylation. Overexpression of human CHIP, a zinc-independent E3 ubiquitin ligase that targets p53, relieved TPEN-induced p53 stabilization and reduced apoptosis. Expression of p53 pro-apoptotic target genes was upregulated by zinc deficiency. Correspondingly, embryos cultured with p53 transcriptional activity inhibitor pifithrin-α could overcome TPEN-induced apoptosis and failure of neural tube closure. Our studies indicate that zinc deficiency disrupts neural tube closure through decreased p53 ubiquitylation, increased p53 stabilization and excess apoptosis.” (Li, Zhang, Niswander, 2018)
Or, the neural tube may have closed, but then zinc deficiency related apoptosis (Li, Zhang, Niswander, 2018) caused some of the brand-new cells to die and the closure may have reopened.
“The development and closure of the neural tube is completed 28 days after conception. If neural tube closure fails, the embryo develops an NTD. However, some authors also support the possibility of some NTD resulting from a closed neural tube secondarily reopening [21].” (Imbard, Benoist, Blom, 2013)
Zinc deficiency is not uncommon and might be more likely in someone who isn’t eating well due to hyperemesis. Low zinc intake is more of a risk for vegans. Meats and shellfish are good or excellent sources. Pumpkin seeds, other seeds, nuts and beans, have some zinc. Dairy products, milk and cheese, are also a source of zinc, not as high as in meats but more bioavailable than the zinc in plant foods. Minerals can be bound to phytonutrients and less absorbable for us. (healthline/zinc)
Disclaimer: Opinions are my own and the information is provided for educational purposes within the guidelines of Fair Use. While I am a Registered Dietitian this information is not intended to provide individual health guidance. Please see a *functional health professional for individual health care purposes.
Reference List
(Amagloh, et al., 2017) Amagloh FK, Atuna RA, McBride R, Carey EE, Christides T. Nutrient and Total Polyphenol Contents of Dark Green Leafy Vegetables, and Estimation of Their Iron Bioaccessibility Using the In Vitro Digestion/Caco-2 Cell Model. Foods. 2017 Jul 22;6(7):54. doi: 10.3390/foods6070054. PMID: 28737681; PMCID: PMC5532561. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5532561/
(Digitale, med.Stanford.edu/news) Digitale, E., Low choline levels in pregnant women raise babies' risk for brain and spinal-cord defects, study shows, Aug. 12, 2019, med.stanford.edu, https://med.stanford.edu/news/all-news/2009/08/low-choline-levels-in-pregnant-women-raise-babies-risk-for-brain-and-spinal-cord-defects-study-shows.html
(Imbard, Benoist, Blom, 2013) Imbard A, Benoist JF, Blom HJ. Neural tube defects, folic acid and methylation. Int J Environ Res Public Health. 2013 Sep 17;10(9):4352-89. doi: 10.3390/ijerph10094352. PMID: 24048206; PMCID: PMC3799525. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3799525/
(Irvine, et al., 2022) Irvine N, England-Mason G, Field CJ, Dewey D, Aghajafari F. Prenatal Folate and Choline Levels and Brain and Cognitive Development in Children: A Critical Narrative Review. Nutrients. 2022; 14(2):364. https://doi.org/10.3390/nu14020364 https://www.mdpi.com/2072-6643/14/2/364
(Li, Zhang, Niswander, 2018) Li H, Zhang J, Niswander L. Zinc deficiency causes neural tube defects through attenuation of p53 ubiquitylation. Development. 2018 Dec 13;145(24):dev169797. doi: 10.1242/dev.169797. PMID: 30545932; PMCID: PMC6307889. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6307889/
(Rao, et al., 1998) Rao PV, Garrow TA, John F, Garland D, Millian NS, Zigler JS Jr. Betaine-homocysteine methyltransferase is a developmentally regulated enzyme crystallin in rhesus monkey lens. J Biol Chem. 1998 Nov 13;273(46):30669-74. doi: 10.1074/jbc.273.46.30669. PMID: 9804840. https://www.jbc.org/article/S0021-9258(19)59286-9/fulltext Figure 6.
(Sbodio, Snyder, Paul, 2018) Sbodio JI, Snyder SH, Paul BD. Regulators of the transsulfuration pathway. Br J Pharmacol. 2019 Feb;176(4):583-593. doi: 10.1111/bph.14446. Epub 2018 Aug 23. PMID: 30007014; PMCID: PMC6346075. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6346075/




